 Joan MV Pons, Head of Evaluation AQuAS
Joan MV Pons, Head of Evaluation AQuAS
In 2007, a high interest health economics research article was published and promoted by the Department of Health1. The study broadcasted the public health care budget for 2005, not only for the 17 categories of the International Classification of Diseases (ICD), but also by the type of assistance and mainline services. There is no doubt that the work provided a reference point for health planning and management and offered an unexpected surprise as, until recently2, the newer data of this kind and obtained using a similar methodology was not being made public. I admit that it has been a personal interest of the Minister to see the data presented in this manner.
And in this interval, 2005-2015, what do the numbers say, more exactly, the euros? First, let’s have a look at the overall graphics and then at its sections.
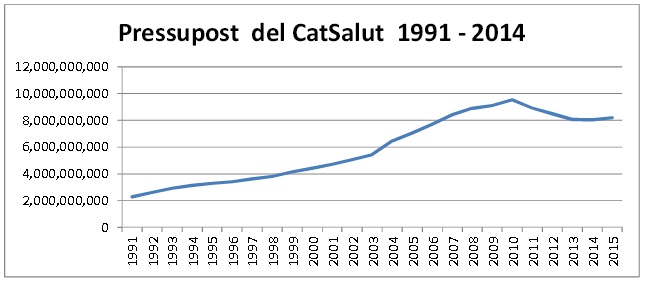
Let’s start by mentioning that the harsh cuts timeframe was in 2011-2013 when CatSalut’s budget had to be reduced by 1.5 billion Euros compared to 2010, the year when this expenditure (or investment for some and certainly a source of health and financial benefits for many people) reached its peak. Worthy of mentioning is that between 2003-2010, CatSalut’s budget growth far exceeded the GDP growth, but this was a very common trend before the crisis. We will not go along with littleness, by asking whether, despite the reduction in public spending, the budget for social policies (health, education, welfare and family) of the Catalan government has increased in percentage within Catalonian budgets (71.2% in 2015). Accurately, the 2005 health budget represented 40% of the Catalan public budget and in 2015 we have the same percentage, but the amounts are very different. Here we could apply the phrase attributed to both Mark Twain and Benjamin Disraeli regarding the three types of lies: lies, damned lies and statistics.
If we continue down the broad lines of services, we have to study them with graphics such as the following (pressupost = budget):

If we examine the budget distribution among major areas or major lines (functional classification) we notice striking things worthy of mentioning. The first, undoubtedly, is the reduction in pharmacy spending that has reached stratospheric levels in the mid of the last decade, (almost 24% of all health care budget). Plenty of measures with regards to the quality of prescribing have been implemented, from the most effective in price levels and generic to the more educational (professional) and motivating (management by objectives). It’s clear that for many years, the local and foreign pharmaceutical industry, existed in a cloud due to the lack of a genuine public pharmacy policy in this country. For this reason, those covenants that demanded returns of profits with which research networks (ISCIII) were financed and, amusingly, funds for activities aimed at rational drug use that the Ministry distributed among nationalities and regions, emerged.
Therefore the pharmacy spending goes down (as the return of the pharmaceutical industry to research and rational use), but the more particular pharmacy, the high technology pharmacy (biotechnology, whether medicine of recombinant origin or monoclonal antibodies) as is the MHDA (ambulatory drugs dispensed at the hospitals), continues to rise with an absolute increase of 61.6% between 2005 and 2015 (from M€390.29 to M€630.93). A more thorough analysis of the changes in pharmaceuticals expenditure, whether in a hospital or for distribution to outpatients, would force us to examine in more detail the different types of drugs and their use.
We can also notice an increase in spending on health care, both primary and specialized, as the latter grows much more to represent more than half (58%) of public insurance spending. The trend of focusing on hospitals and unrestrained specialized care also comes from afar. We may say, although without the data, that there is an incipient turnaround in recent years, of a slight decrease in specialized care and slight increase in primary care. The growing need for attention to chronic disease and for integration of social services (health and social care), the two sides of the same coin, should go on shifting this situation.
1 Gisbert R, Brosa M, Bohigas L. Distribución del presupuesto sanitario público de Catalunya del año 2005 entre las 17 categorías CIE-9-MC. Gac Sanit 2007;21:124-31.




