SUSTAIN is a Horizon2020 European Project related to integrated care for older people that live at home with complex health and social needs. Thirteen initiatives from seven European projects participate in it.
SUSTAIN is a Horizon2020 European Project related to integrated care for older people that live at home with complex health and social needs. Thirteen initiatives from seven European projects participate in it.
It is a project whose aim is to improve a range of things including the care centred on the individual, the coordination of teams of professionals, the preventive nature of care, safety and efficiency.
In Catalonia, two initiatives (Social and Health Integration of Sabadell Nord and the Programme for complex chronic and advanced patients and the geriatric population of Osona) have participated in the design and development of projects for improvement which have been assessed by AQuAS (you can read the report and article here).
On 23rd January, 2019, professionals involved in the groups that are the driving force of the two local initiatives (Sabadell and Osona) of integrated health and social care – family doctors, workers and social workers, nurses, geriatric and management personnel- met at AQuAS in their first joint meeting.

The professionals were able to share thoughts on one question: What remains of the SUSTAIN project in the territory?
This was the starting point to identify specific actions that can make the projects sustainable and to also comment on aspects for improvement beyond the projects.
The aim was to identify opportunities within reach of the local initiatives themselves that could serve to generate a more favourable environment for integrated health and social care centred on the individual, both preventive and reactive in nature.
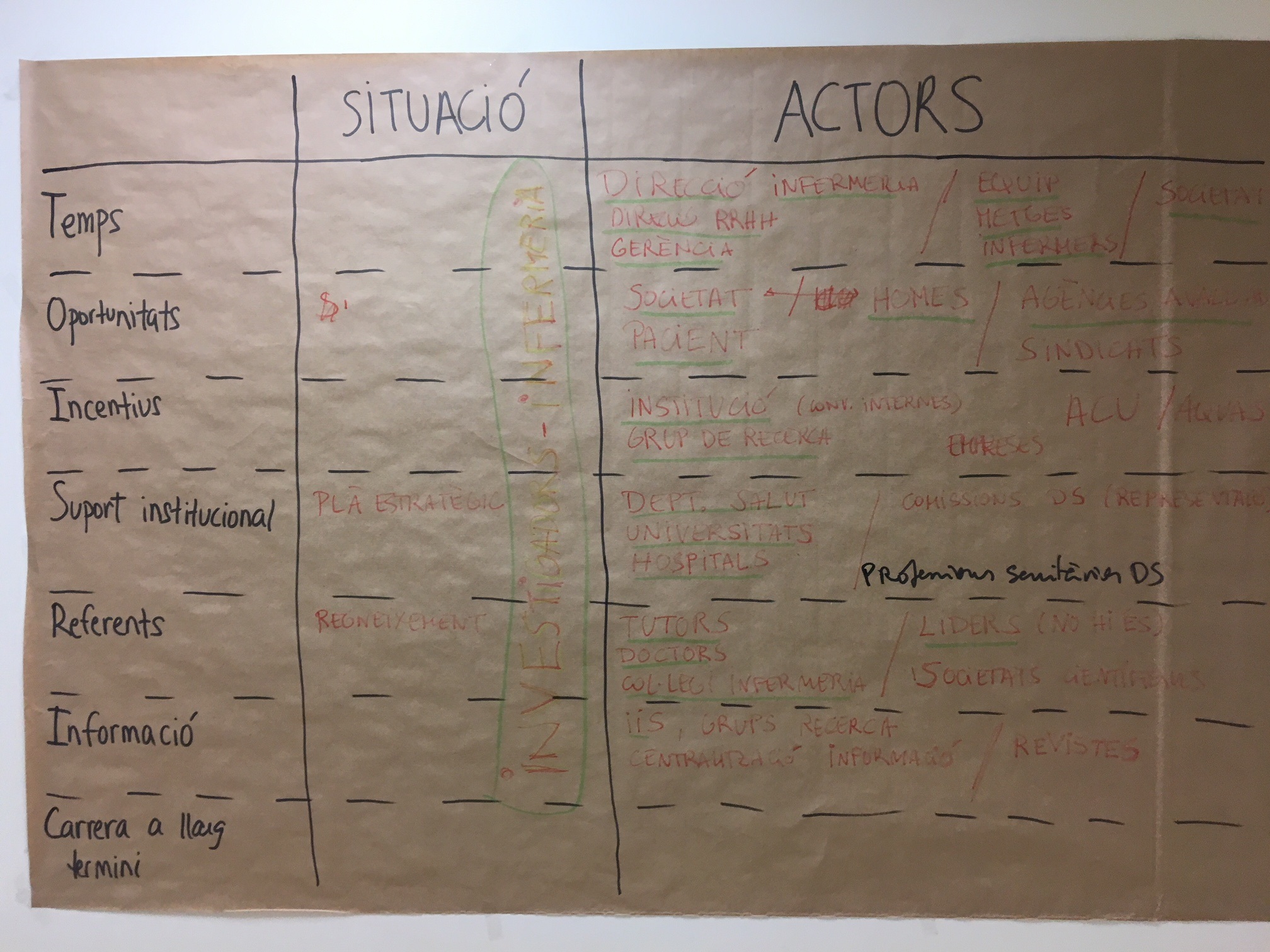
From the brainstorming that was done, a multitude of local actions can be derived with which to drive integrated health and social care centred on the individual. Let’s look at it in detail:
- Prioritise at a population level Delimiting a population group for which it is deemed most important to apply the new PIAI method (Individualised Plan for Integrated Care), so that efforts can be concentrated on this group until the context allows for scaling up to the entire population of 65 and older. One possibility would be the older people who live at home with complex health and social needs who at present receive home-based healthcare, or for those cases known by primary healthcare but are not beneficiaries of home-based social care. This would be done in order to eliminate the barrier limiting access to social services or because there is a lack of awareness of these social service
- Provide continuity in coordination between sectors, while taking into consideration the suitability of the new PIAI method for each individual case Continuing with periodic meetings of the team of professionals in charge of the multidimensional assessment of needs so as to plan an individualised and integrated health and social care (at least of the triad of primary care, family medicine-nursing-social work). These meetings, held on a monthly basis, would enable the teams to consider who, among those users visited recently (in primary care centres, at home, at local social services, at intermediary care in the case of Osona), would particularly benefit from the integrated and participative approach of SUSTAIN, with the possible introduction of changes or objectives to improve their care and their quality of life.
- Inviting professionals that have not participated in SUSTAIN to use the new PIAI method, giving these professionals the necessary tools (time, training) so they can familiarise themselves with the approach of integrated health and social care centred on the individual. With this in mind, there is talk of the importance of “maintaining the spirit of SUSTAIN” and in gradually getting the most reluctant professionals more involved in introducing changes to their way of working.
- Carrying out an analysis of the different capacities and responsibilities of each professional in primary care teams (family medicine-nursing-social work-social health work), and sharing out roles and responsibilities ad hoc, which can enhance the skills of each individual. This could mean that professionals who officially occupy the same position (for example, family medicine) would become specialised in one or another type of care (emergency, development of the PIAI, specific pathologies), and it would mean accepting that not all professionals with the same position need do the same: “one-size-only professionals are not needed”.
- Enhancing the figure of the spokesperson in a healthcare team, both when dealing with a user as well as an internal coordinator of a team, emphasising that the user has a team with professionals that interact with each other in order to provide solutions to their different needs as quickly as possible. The emphasis is on the opportunity that workers and social workers have in acting as liaison officers between primary care, local social services and community resources while at the same time coordinating actions which are contained in the PIAI.
- Analysing how the figure of the social and health worker can best fit in In the case of Sabadell, this figure has only been incorporated very recently. An analysis will need to be carried out with the entire group of professionals that intervene in care but especially with the social workers (under contract with local social services, socio-health workers or social workers specialised in intermediary care). This will be done in order to understand their capacities and perspectives of what function each professional should have bearing in mind their particularities and the specific environments in which they work (for example, specific tools and procedures they can apply, what information systems they have at their disposal or what other professionals they are in direct contact with).
- Set up safe and respectful local systems with the LOPD (Spanish personal data protection law) in order to exchange the minimal information necessary to carry out a joint multidimensional assessment and to share the PAIAs among the most important professionals in each case. The example of Integrated System of Health in Osona (SISO) is mentioned, which enables primary care professionals to see which users are admitted in the hospital centres that make up the system, or the mechanism foreseen by the County Council of Osona to enable social health workers employed in health centres to consult the degree of dependency of a user.
We end this post by commenting that this week we participated in the final conference of the project in Brussels.

Post written by Jillian Reynolds, Lina Masana, Nuri Cayuelas and Mireia Espallargues.